1
Volunteer
Handbook
2
Welcome to Adventist Health Glendale
Thank you for your interest in seeking a volunteer opportunity at
Adventist Health Glendale. We welcome enthusiastic individuals of
all backgrounds and abilities and are committed to providing equal
opportunity for all applicants who wish to volunteer at our hospital.
Contact Us
Volunteer Services Department
(818) 409-8057
ahglvolunteerse[email protected]
Volunteer Services is located on the Main Floor of the East Tower.
The office is open from:
• 8 a.m. – 4:30 p.m. Monday/Wednesday/Friday.
Please email us to make an appointment if you would like to visit our office.
Please do not hesitate to contact the volunteer department if you
have any questions or concerns.
Table of Contents
3
About Adventist Health Glendale 5
Our Mission and Values 5
The Volunteer Department 6
Volunteer Policies 6
Volunteer Hours 6
Volunteer Benefits 6
Getting Started 8
Application Process 8
Interview 8
Background Check/Drug Test 8
Immunizations 8
Annual Volunteer Requirements
Annual TB Evaluation Test 9
Annual Flu Shot 9
Annual Review of Policies and Procedures 9
Personal and Emergency Contact Information 9
Verification of Volunteer Hours 9
Placement Restrictions 9
Relatives of AGHL Employees 9
AHGL Employees 9
Teens 10
Illness/Significant Loss Leave 10
Volunteer Orientation 10
Uniform and Appearance 10
Volunteer Placements 11
Additional Procedures and Requirements 11
Signing In and Hours of Credit 11
Benefit Hours 11
Parking 11
Cell Phones and Electronic Devices 11
Meal Breaks 11
Attendance Policy 12
Reasons for Termination 12
Transfers 12
Grievance Procedure 12
Disability or Workman’s Compensation 12
Acceptance of Tips 13
4
Standards 13
AIDET 13
Working with Patients 15
Conversations 16
Entering rooms 16
Volunteers May Not 16
Transport 16
Wheelchair Protocols 17
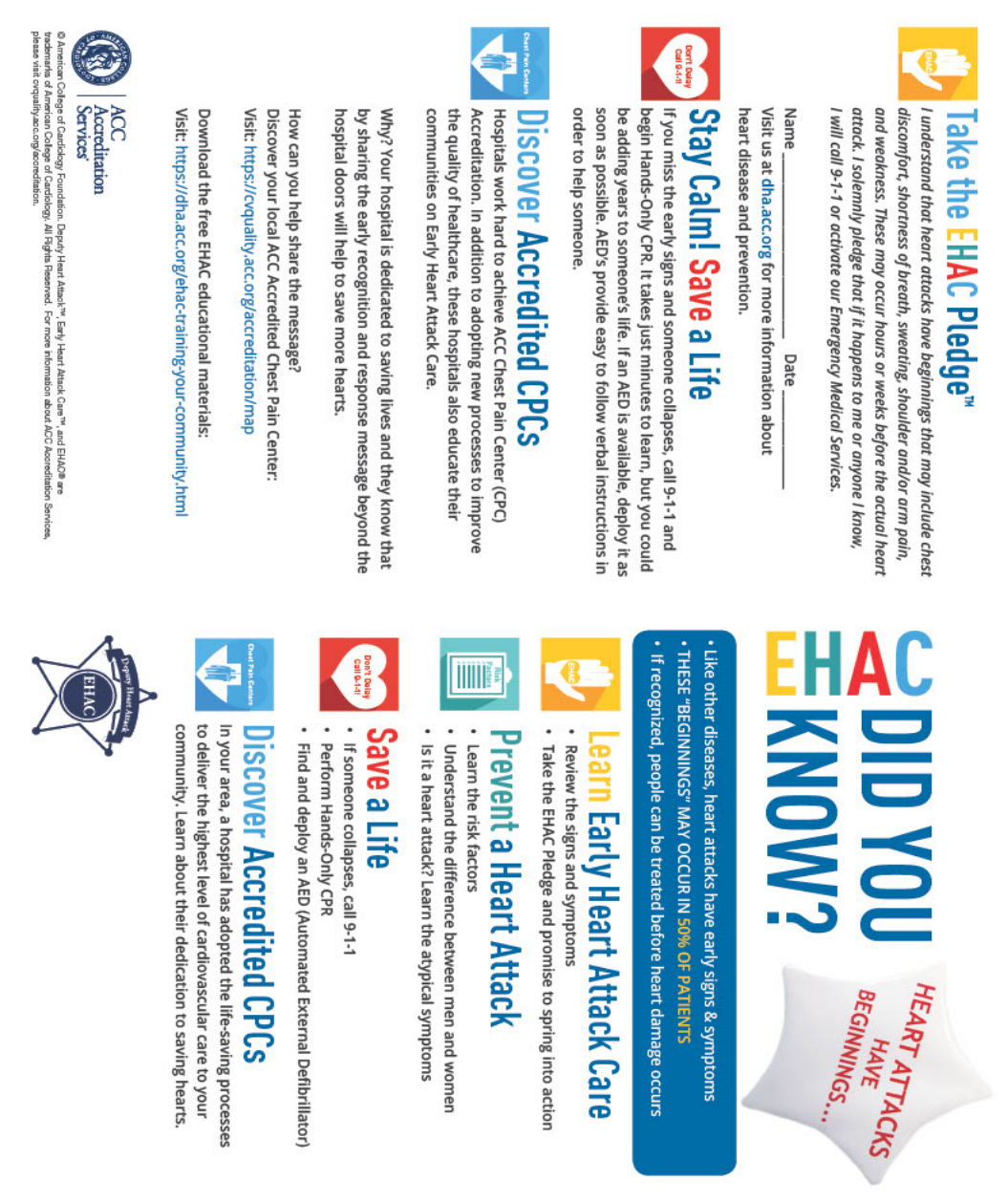
Early Heart Attack and Care 18
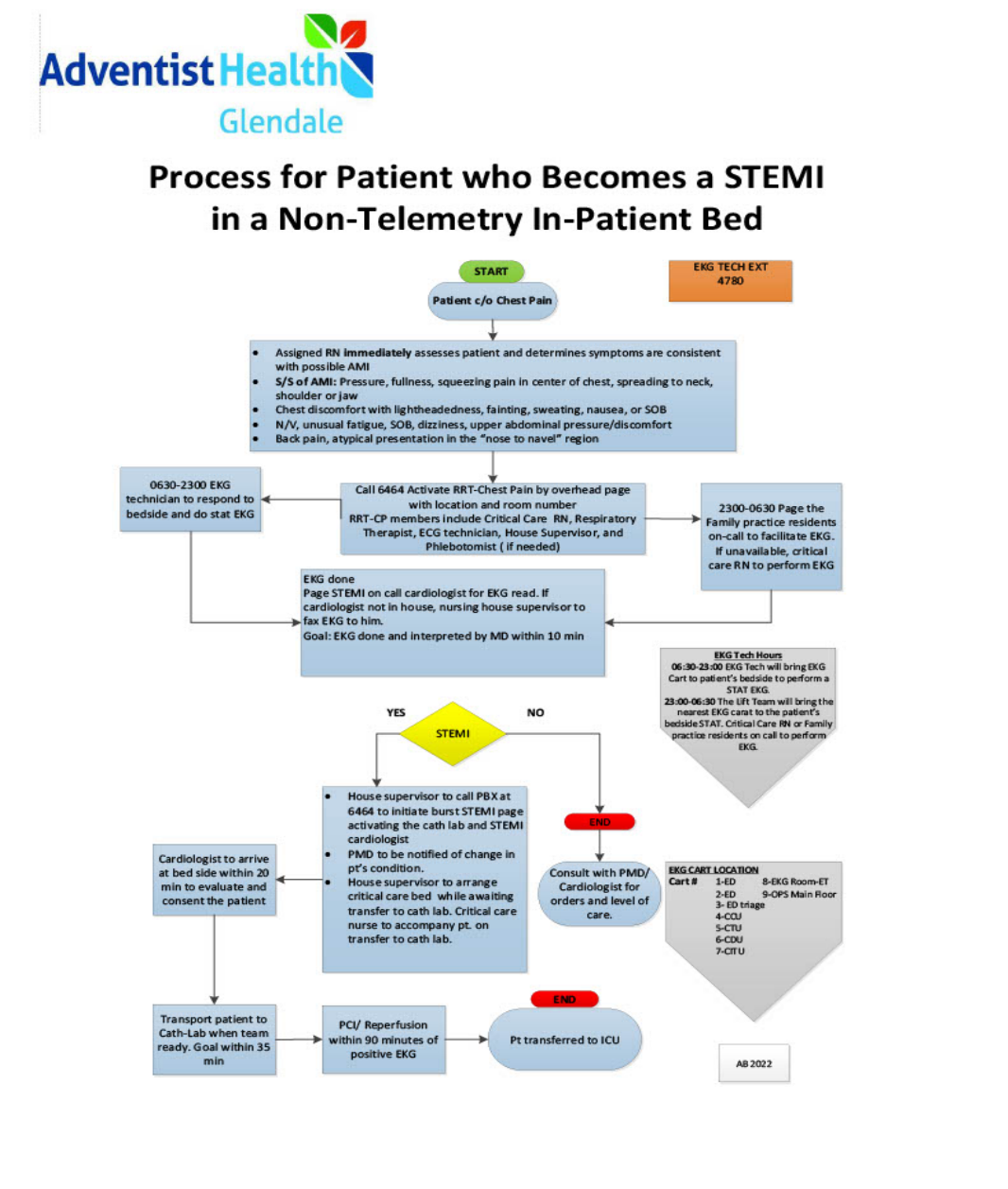
Process to Seek Assistance for Cardiac Emerg. 20
Adventist Health Privacy Policies 21
HIPAA 21
HITECH 21
Social Media 22
Protected Health Information 22
Patient Rights 22
Consequences of Noncompliance 23
Reporting Violations 23
Hospital Safety 23
Handwashing 23
Infection Control 24
Pathogens 24
PPE protection 25
Volunteer Safety 25
Emergencies
Emergency Codes 26
Fire Safety 27
How to Use a Fire Extinguisher 28
What Causes Fires 28
Fire Evacuation Routes and Procedures 29
Evacuation and Patient Priorities 29
Disaster Plan Policy 29
Workplace Protocols 30
Health Requirements 31
Campus Map 32
5
Adventist Health Glendale Mission and Values
Our Mission
Living God’s love by inspiring health, wholeness and hope.
Our Values
• Be love: Love matters. Treat yourself with love and care so that you are free to love and care for
others.
• Be trustworthy: Forgive freely and find common ground.
• Be a force for good: Be courageous. Take action. Whether it is through your position or your
passion, work to impact your community for the better.
• Be a mission owner: Own your role, find your talent and know that your contribution is mission
critical. Ask yourself, “How do I inspire health, wholeness and hope?”
• Be welcoming: Recognize all people are created equal and embrace them in hospitality as you
would a cherished friend.
• Be curious: Seek to understand how things work and why. Innovate and be open to new ideas
and approaches. Own your mistakes and learn from them.
• Be brilliant: Leverage your best talents and skills to shine. Make promises and keep them.
Always expect the same from others.
Our Vision
Compelled by our mission to live God’s love by inspiring health, wholeness and hope, we will transform
the health experience of our communities by improving physical, mental and spiritual health; enhancing
interactions; and making care more accessible and affordable

6
The Volunteer Department
Policies:
• AHGL volunteers work under the direction and supervision of paid staff and do not earn or
collect a salary from the hospital, or department where they volunteer.
• Volunteers are not permitted to accept money from grateful patients or their families.
• AHGL also does not train volunteers for employment or paid positions within the medical
center.
• If a volunteer applicant is interested in a paid position she or he should visit the job opportunity
page on AHGL’s website at: https://www.ahsocalcareers.com/
• All Volunteer assignments must be authorized by the Volunteer Department.
• Volunteers are assigned to specific departments by the Volunteer Department to perform tasks
for which they have been authorized by a nurse manager, supervisor, or coordinator to perform.
• Volunteers are not permitted to perform any type of invasive procedures such as drawing blood
or giving injections; and they are also prohibited from performing any task that requires a
license or certification.
• Procedures that require a license or certification may only be performed by AHGL paid
employees.
Volunteer Hours:
• Adult Volunteers are expected to commit to 100 hours in a continuous 12-month period. Adult
Volunteers must volunteer a minimum of 4 hours a week with a maximum of 16 hours a week.
• College Volunteers are expected to commit to 100 hours of volunteering per academic year.
College Students must volunteer a minimum of 4 hours a week with a maximum of 16 hours a
week.
• High School Volunteers are expected to commit to 60 hours of volunteering per academic year.
High School students must volunteer a minimum of 2 hours a week with a maximum of 8 hours
per week.
Volunteer Benefits:
Volunteers will receive 1 meal or 1 snack per day depending upon hours worked. Volunteers will also
receive free parking. Volunteers are recognized at events in appreciation of volunteer participation.
Volunteers who complete 100 hours of service (and for every 250 hours thereafter) will receive special
recognition during Volunteer Appreciation Week. Volunteering is a great opportunity for earning hours
for school or community service
7
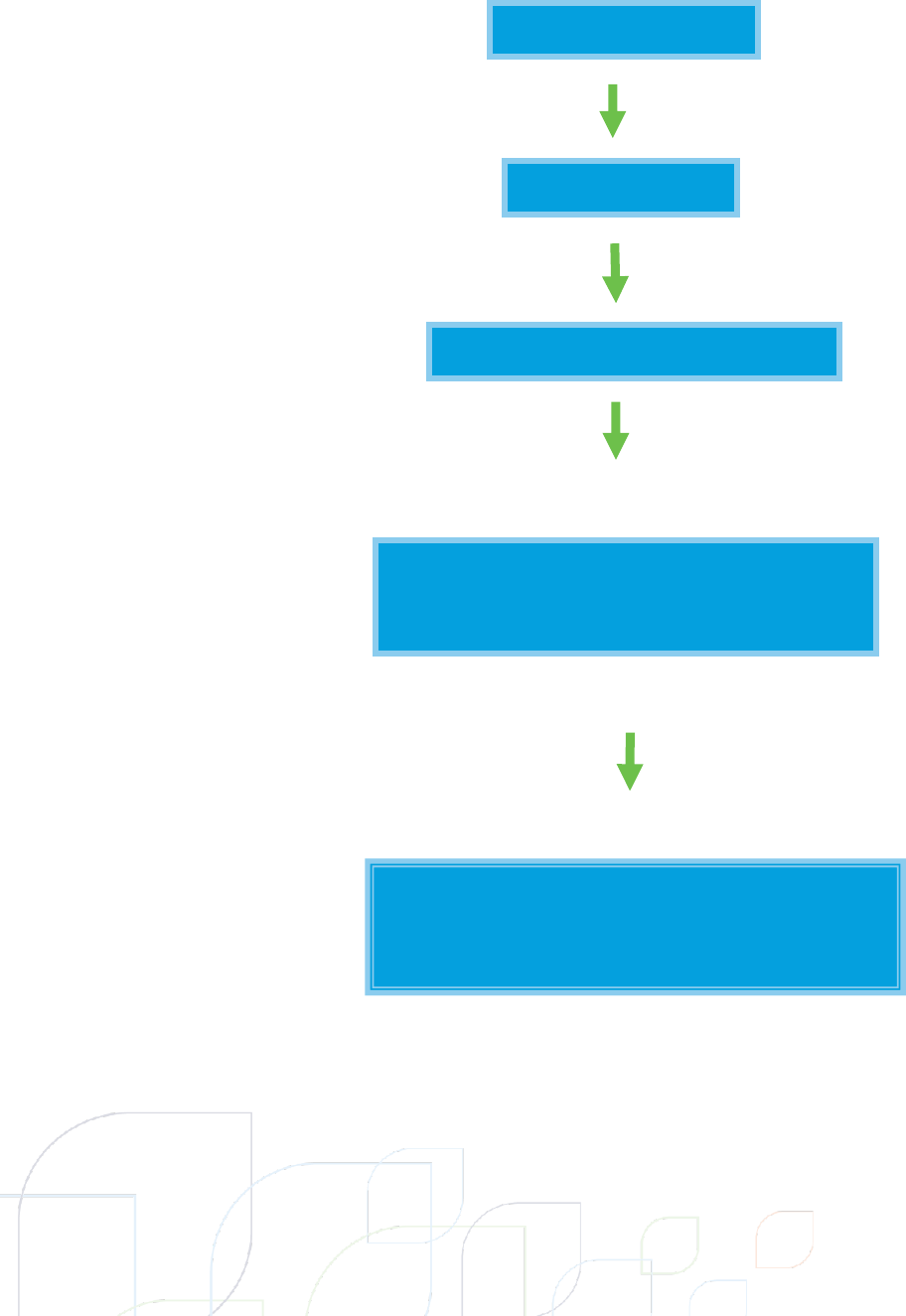
ORGANIZATIONAL CHART
Unit Manager/Director
Board of Directors
President
VP Business Development
Manager
Volunteer Services Department
Volunteers
Program Participants
8
VOLUNTEER HANDBOOK
GETTING STARTED
In order to become a new Volunteer, there are several steps that must be taken which are set
forth by the hospital.
Application
All Volunteers are required to submit a volunteer application. High School students will need to submit a
letter of recommendation from either a high school teacher or counselor. Once the application is
submitted and reviewed, applicants will receive an email from the Volunteer Supervisor with next steps.
Placement Interview
Volunteer applicants will be interviewed by the Volunteer Services Manager. During the placement
interview process, the desire or need to volunteer will be discussed, along with any experience or
qualifications the applicant may have. This discussion will help us to determine an appropriate
assignment and schedule for the applicant.
Background Check & Drug Test
Volunteers 18 years old and older must submit authorization for a background check, which is provided
by Adventist Health Glendale (AHGL). All applicants will need to pass a drug test. (Occupational
Medicine)
Immunizations
Applicants who have passed the interview stage of the applications process must provide proof of
immunizations. Volunteers must show proof of a Tdap or Tetanus shot within the last ten years.
TB Test
All volunteers are required to complete a two-step tuberculosis (TB) skin test. The first step is given after
the placement interview and the second test will be given during Orientation. Applicants who have
received a negative TB skin test in the past year will only need to provide proof of immunization for one
additional TB prior to the start of Volunteering. If a TB test turns out positive, the applicant will need to
receive a chest x-ray. Volunteers may not start volunteering until they have received TB clearance. TB
tests are FREE if administered by the hospital’s Employee Health Department.
Flu Shot
All Volunteers are required to submit proof that they have received an annual flu shot. Flu shots are
FREE if administered by the hospital’s Employee Health Department during flu season (September –
April). If an applicant is allergic to the flu shot, a doctor’s note on official letterhead must be submitted
along with their application. Volunteers who are allergic to flu vaccine must wear masks during flu
season. Volunteer who decline the flu shot will also be required to wear a mask while on AHGL campus.
MMR and Varicella
9
All volunteers must show proof of 1st and 2nd MMR and Varicella vaccinations from childhood prior to
volunteering. If applicant does not have access to childhood records, applicant must submit proof of 1
MMR and Varicella immunization as an adult. Blood titers indicating immunity to MMR and Varicella are
also accepted if the volunteer does not have the official dates of vaccination.
Orientation
All Volunteers must attend an Orientation session held once a month in order to begin Volunteering.
The Orientation will cover AHGL policies and procedures and expectations, as well as a tour of the
hospital. Volunteers must bring their immunization records to the Volunteer Office prior to Orientation.
Employee Health must approve Volunteer health histories in order to receive their hospital badge.
VOLUNTEER HANDBOOK
DEVELOPMENT POLICIES
All Volunteers must renew their annual flu and tb immunizations each year in order to continue
volunteering. All Volunteers will also be required to complete Health Stream Education Modules once
each year to review AHGL policies and any additional updates to the Volunteer program. Failure to
comply with the annual requirements will result in termination from the Volunteer program. Volunteers
are responsible for updating their personal contact information and Emergency contacts if information
changes.
Verification of Volunteer Hours
Written verification of Volunteer Hours will only be provided upon completing the required number of
hours.
Placement Restrictions
In order to protect the professionalism of AHGL, there are certain restrictions on where Volunteers may
be placed.
Relatives:
Volunteers may not be placed in a Department:
• Where a relative is employed including family, in-laws and/or step-family members.
• Where a relative directly or indirectly supervises the Volunteer
• Where a placement would violate internal control between Departments
• Any other relationship that the Department Head considers detrimental to the operation of the
Department and the hospital (e.g. with a significant other)
AHGL Employees Only:
AHGL Employees may not Volunteer in the same department where they are employed and must be
placed in a Department with a different Department Manager/Supervisor than their job.

10
Teens:
Teen Volunteers may not visit, observe or volunteer in the Emergency Department, Surgery and Critical
Care.
Illness/Significant Loss:
Placement restrictions may be placed on Volunteers with independent circumstances such as an illness
or significant loss regarding where they may Volunteer or when they can begin Volunteering.
Such circumstances may include:
• Volunteering in a department where the Volunteer themself is a recurring patient
• Volunteers with recent health problems that require time away from the hospital and/or patients
• A minimum of 3 months post-discharge from the hospital before Volunteering
• A minimum of 1 year must pass for Volunteers who have had a significant grief loss experience before
working with patients at AHGL
• At least one year of cancer remission is required for Volunteers who have had a cancer diagnosis.
Volunteer Orientation
New Volunteers must attend a mandatory orientation as part of the onboarding process. Orientations will be held
once a month during the week. Orientations will review Volunteer expectations, hospital policies and procedures
and include badge receivals and a hospital tour. All Applicants are required to have their completed immunization
forms ready and approved before orientation in order to receive a badge and start volunteering. Any Volunteers
who are not able to begin volunteering within 3 months of orientation will need to schedule a new interview and
participate in a second orientation.
Uniform and Appearance
Volunteer badges given by Volunteer Services are part of the uniform and must be worn and visible at
ALL times when volunteering. If a Volunteer forgets their badge, a temporary badge from Volunteer
Services must be requested before starting their shift.
Volunteers must wear proper uniforms during all Volunteer shifts. Uniforms are comprised of an official
AHGL shirt and black slacks with no rips or tears. No jeans or shorts are allowed at any time in any area.
*Scrubs are only acceptable if required in the Volunteer’s assigned area. Volunteers must check in with
their department supervisor and obtain explicit approval before wearing scrubs.
Clothing must be clean, well-fitting and wrinkle-free. Under garments must be worn at all times.
Unacceptable clothing includes: tight fitting garments, shorts, skirts, sweat pants, capri pants, leggings,
athletic wear, denim, sheer or crochet type fabrics, caps and backless, sleeveless, spaghetti strap, halter,
or tube tops.
Closed-toed shoes must be worn while volunteering. No backless shoes. Socks must be worn at all times.
Shoes must be tied. Flip-Flops, beach shoes, deck shoes, high heels and slippers are unacceptable.
Clean hair, nails and clothing are very important in the health care setting. Volunteers should avoid
wearing heavy, colorful makeup and wear light, “natural” makeup. All Volunteers should wear
deodorant and avoid excessive use of perfume, cologne and after-shave lotion. Long hair must be tied
back and secured. Facial hair must be neat, clean and trimmed. Artificial nails are not to be worn in
11
patient care areas. Polish should not be chipped and should not have any nail “jewelry”. Nail length is
not to interfere with the job or pose a hazard to the patient or another employee.
Small sized jewelry is acceptable. Elaborate or large jewelry is not appropriate. Nose or other facial
jewelry is not acceptable. Visible body piercings are not to be worn while on duty, except for the ears.
Visible tattoos should also be covered while volunteering.
No gum chewing is allowed while volunteering. Volunteers must be professional and appropriate at all
times.
Additional Procedures and Requirements
Signing In and Hours of Credit
All Volunteers must sign in and sign out every time you Volunteer at AHGL. Sign in iPads are located
throughout the hospital. Use your AHGL ID badge to sign in and out. When you arrive in the area of your
assignment, check in with the person in charge of the department. During volunteer hours, always
inform the person in charge if you are leaving the area for any reason. When you have completed your
shift, inform your supervisor that you are going off duty. Make sure that you do not sign out until you
are ready to leave. Complete and accurate attendance records are essential for security purposes and
are necessary for the protection of the volunteers in case of emergency, as AHGL is liable for everyone
on hospital grounds. Signing in and out also tracks your volunteer hours. You will not receive any credit
for hours that are not logged in the AHGL computer system.
Parking
Volunteer badges will allow access into designated parking structures. Volunteers will be allowed to park
in the structure and receive a validation at the end of their shift.
Cell Phones and Electronic Devices
Cell phones and electronic devices may not be used while volunteering. Volunteers may only use
personal electronics during break times and in non-public and non-work areas of the hospital. Family
members may call the Volunteer Department office if there is an emergency. AHGL prohibits the use of
cell phone features including camera, video and audio in order to protect patient privacy. Headphones,
earphones or ear buds are never to be worn in the hospital. Volunteers who break this policy will receive
a warning. If a Volunteer receives three warnings, they will be terminated from the volunteer program.
Meal Breaks
Meals and snacks may not be eaten except in designated areas, like the Terrace Cafeteria, Anniversary
Garden and the Volunteer Resource Room. Food is prohibited in patient care areas, lobbies and other
work areas. Volunteers receive vouchers to use in the Cafeteria. Volunteers who work 4 hours receive a
snack voucher. Volunteers who work 8 hours receive a meal voucher.
Attendance Policy
If you are sick, do not come to the hospital to volunteer because you can infect someone else. If you are
scheduled, please call your supervisor to let them know you won’t be there for your shift. They are
relying on you, so please do not be a no-show, no call. Make sure to give as much notice as possible if
arrangements need to be made to bring in another Volunteer in your absence. If you are going to be
12
late, please call the department and let them know. If you have 3 unexcused absences, you will be
terminated from the program.
You must inform your department, and the Volunteer Office ahead of time if you need a leave of
absence. If you will be taking the summer off or if our records indicate you have not been volunteering
for more than 90 days, Volunteers will be inactivated and are required to re-apply. You must turn in your
ID badge in to the Volunteer Services office before your leave.
**ALL Volunteers must return their hospital badge and uniform when finished with their service.
Reasons for Termination
Volunteers may be terminated for the following reasons:
• 3 unexcused absences
• Not fulfilling weekly time requirement
• Not completing total time commitment
• 3 month absence without taking a “Leave of Absence”
• Falsifying health records
• Outdated health records (Annual TB and annual flu)
• Not notifying department when sick or late
• Not showing up on scheduled days, or showing up on unscheduled days
• Falsifying hours
• Failing to comply with uniform codes after two warnings have been given.
• Accepting tips from patients or visitors
• HIPAA violation
• Working in a department where a Volunteer is not trained for or does not have badge clearance
If a Volunteer is terminated, they must turn in their ID badge and uniform to the Volunteer Office in
person.
Transfers
Volunteers who wish to transfer to another Department must speak to their supervisor and the
Manager of Volunteer Services. It is expected that the Volunteer spend at least three months in their
current position before transferring because of the specific training required for each Department.
Grievance Procedure
Volunteers should take all suggestions and complaints to their immediate supervisor first. If the
Volunteer remains unhappy with the resolution, they may speak to the manager of their Department or
the Manager of Volunteer Services, who has the final say over any unresolved issues.
Disability of Workman’s Compensation
Volunteers who receive disability or workman’s compensation benefits MUST bring a written statement
from their physician on official letterhead to the Volunteer Department stating their work status and
specific restrictions.
13
Acceptance of Tips
Volunteers may never accept tips from patients or visitors. Accepting tips is a violation of AHGL hospital
policy. Volunteers who are caught in violation of this policy will be terminated from the program.
Standards and Patient Experience
AIDET
Acknowledge
Identify
Duration
Explain
Thank You
AIDET is a communication technique that reminds us of the fundamental elements patients and family
members need to decrease their anxiety and build trust with us as caregivers. AIDET improves
compliance for better outcomes because patients will cooperate more readily with their plan of care as
a result of that trust. AIDET ensures that we are providing clear communication – which creates a safe
environment to receive care. AIDET helps us build loyalty so we can be a trusted and preferred
healthcare provider of choice.
Communication
AIDET is at the heart of providing an environment in which excellent patient care can provided. Be
aware of who your customers are. Visitors are our guests and expect to be treated with respect and
courtesy, and to receive assistance in an efficient and appropriate manner. Practice AIDET when
interacting with patients, their families, visitors, employees and other Volunteers.
Acknowledge the patient. Greet them and offer assistance, help them solve their problems, and
welcome them to come to you again if they need anything else. For patient care interactions, use the
following:
• Offer a greeting when passing, such as, “Good morning” or “Good Afternoon”.
• Connect with the patient and family members by addressing them as Mr./Ms., or by the name
that they prefer.
• Smile, make eye contact and greet everyone in a pleasant manner.
• Allow patients and visitors to go first when getting in/out of elevators, doorways and in the
hallways.
• Listen with compassion and understanding.
• Nod when listening to show you are engaged.
• Answer their questions professionally and with competence.
Introduce yourself and your role to patients, visitors, and other hospital staff.
• Tell them that you are there to provide assistance, and let them know what you can do for
them.
14
• Offer to help visitors get to their destination, or provide directions.
Duration
Wait times may cause stress for patients and their families. As a volunteer you are not authorized to
share information regarding the amount of time a patient may have to wait for results of a test, or to be
seen by a doctor.
• Communicate with the patient/family the amount of time you can spend with them and that
you will check back with them within 10 minutes or so to see how they are doing and if they
need any further assistance.
• If you are escorting a patient or visitor you may offer an approximate amount of time it may
take to get where they need to go.
Explain how a process works to patients who need help.
It is important that we spend as much time as needed to answer any customer questions or concerns.
Sometimes you may be tasked with responsibilities that include explaining how a process will work. In
other areas you may need to describe a different type of process or provide information, such as our
medical center’s surroundings, of which many visitors may be unfamiliar. Make it a personal effort to
clearly explain or describe how to find what they need if you are not able to escort them.
• Ask and anticipate patient and/or family needs, questions or concerns.
• Respond to patient and/or family questions and requests with immediacy.
Thank patients, families, visitors, hospital staff and other Volunteers for their time.
• Always ask if there is anything else you can do for the patient, employee, visitor, before you end
the conversation or interaction.
• Exit courteously and/or with an explanation of what will come next (or when you will be back to
check on them).
• Say ‘thank you’ anytime anyone does something nice for you such as holding a door or elevator
door open for you, answering a question for you, letting you pass in the hallway, giving you a
compliment or for sharing information with you needed to complete your volunteer task or
project.
• Respond courteously to anyone who says words of thanks to you.
AIDET Phone Etiquette
Often the first impression patients and visitors get from AHGL is through the telephone so it is critical to
make sure that experience is positive. Make sure you identify yourself and the department when
answering the phone. Make certain you write down the message and deliver it promptly. Practice AIDET
phone etiquette during all phone interactions:
• Before answering the phone, discontinue conversations or activities that may be heard by the
caller. Make sure there are no distractions during the phone conversations.
• Answer the phone as soon as possible within 4 rings.
• Identify your department, give your name, and offer assistance such as, “How may I help you?”
Courtesy
Always be courteous whenever patients, family members and visitors are present. This includes the
cafeteria, patient and visitor waiting areas, hallways, elevators, treatment areas and patient rooms.
15
• Speak in moderate tones; be aware of the level of your voice (speaking loudly or yelling) in the
hallways or elevators.
• Avoid lying down, sleeping, removing shoes, using hospital linen, eating, laughing or speaking
loudly or disruptively.
• Avoid boisterous behavior in areas within earshot of patients and visitors.
• Maintain appropriate conversations, being respectful of patient and employee confidentiality.
Conflicts or disagreements of a work-related or personal nature should be discussed where
patients, their families or visitors are not present.
• In order to provide a safe environment of care, speak only English or the language of the
patient/visitor you are helping. Arrange for interpretation services when needed.
• Personal cell phones or listening devices may only be used during break times and only in
designated break areas.
Respect
Respect privacy and dignity.
• Knock on a patient’s door before entering and ask permission to enter.
• Ask permission before examining a patient and provide explanation of the examination or
procedure.
• Do not make disparaging remarks about other departments or staff in front of patients or
visitors.
• Respect individual and cultural differences.
Professionalism
Maintain professionalism in the presence of patients, their families, visitors or co-workers.
• Show pride by maintaining professional appearance while on duty.
• Adhere to organizational appearance standards.
• Wear name badge appropriately.
• Demonstrate an ongoing responsibility and commitment through good attendance and by being
on time to work.
• Demonstrate pride in AHGL by keeping areas clean and safe.
• When within hearing of any patients, family members, visitors or staff members, keep
comments about patients, co-workers, physicians or any part of AHGL positive and appropriate.
Teamwork
Recognize that each person has an area of expertise and that his or her contribution is valuable.
Working with Patients
Conversations
Volunteers should be mindful that conversations should always be positive and noncontroversial.
Volunteers may not give advice or offer opinions even when patients share highly personal information.
Instead, Volunteers should listen with compassion and nod along to show they are listening.
Never discuss your own medical issues with patients or visitors. Volunteers should also never discuss
other patients outside their room. Not only would talking about other patients violate AHGL policy, but
the patients may overhear, even if they appear asleep or unconscious.

16
Entering rooms
Volunteers may enter patient rooms except for ones marked “DO NOT DISTURB” or if there is a
precaution sign on the door. Volunteers should knock before entering, softly address the patient and
listen for an answer.
• Do not enter a room where a nurse is giving treatment, or a doctor is present. If a doctor enters
the room during a visit, the Volunteer should leave immediately.
• Volunteers may never sit on the patient’s bed or place any belongings on the bed.
Volunteers May NEVER:
• Provide food or drinks to patients (Unless directed to do so by nurse/nurse manager)
• Feed patients
• Exchange food items on a patient’s tray
• Handle narcotics
• Give any type of medication to patients
• Sit on or lean on a patient’s bed
• Put belongings on a patient’s bed
• Bathe patients
• Handle bedpans or urinals
• Operate patient equipment that requires technical knowledge
• Change diapers
• Turn or remove patients from the bed
• Raise or lower a patient’s bed without approval from the patient’s nurse
• Change bed linens
• Obtain patient signatures for treatment or medication
• Accept or chart an order or medical instruction for patients
• Disclose ANY confidential information
If a patient asks a Volunteer to do something that the Volunteer is not trained for or instructed to do,
make sure to tell the patient that while you’d love to help, Volunteers are not permitted to perform
those duties.
Transport
When directed to do so, a Volunteer who has received wheelchair usage training may transport patients
by wheelchair as long as they do not have IV’s or other attached medical equipment. Volunteers may
only transport patients by bed or gurney if they are assisting a nurse or a designated hospital employee.
Volunteers may never transport patients by bed or gurney on their own at any time.
Make sure you verify that the patient you are about to transport is the right person by always
confirming the patient’s room number. When entering the patient’s room, ask the patient his/her name
and check the name on the patient’s ID band against the name on the chart.
When you arrive at a destination, never leave the patient unattended. Do not leave until a staff member
has acknowledged receipt of the patient and has taken responsibility for him/her. For discharges, never
leave a patient until someone has arrived to pick him/her up.
17
Wheelchairs
Wheelchairs come in different styles; there is one type with large wheels useful for people to propel
themselves and there is the type which has to be pushed by someone. All chairs have front wheels,
which swivel, brakes, and should always have footrests. It is not difficult to handle a wheelchair. They
roll easily and anyone who is able to walk with ease and has normal strength can handle a wheelchair.
It is of vital importance that the brakes be set before anyone sits down in the chair. They roll easily and
could roll out from beneath the person trying to sit. Use of the brakes is the most important part of
learning to operate a wheelchair.
Footrests are used to keep the patient comfortable and to keep their feet out of the way. Footrests are
removable if you are working in crowded spaces or have to fold the chair for car transport.
There are a number of techniques used in helping patients:
• Have a patient place arms in lap when being transported.
• Push wheelchair from behind, stay close, and put your weight into pushing.
• Avoid slippery surfaces when propelling chair.
• Open doors then back wheelchair through.
• Always take the wheelchair in and out of the elevators correctly and carefully (back the patient
on and off).
• Use caution at corners and doorways
18
Early Heart Attack and Care (EHAC)

19
EHAC (cont.)
20
Process to Seek Assistance for Cardiac Emergencies
21
VOLUNTEER HANDBOOK
PRIVACY POLICIES
Confidential Information
HIPAA The Health Insurance Portability and Accountability Act (HIPAA) is a federal law that requires
Volunteers to:
• Protect the privacy of patient information
• Secure patient health information in physical and electronic form
• Adhere to the “minimum necessary” standard for use and disclosure (i.e., sharing) of patient
health information
HITECH
The Health Information Technology for Economic and Clinical Health Act
HITECH requires Adventist Health to report breaches of patient privacy to the Secretary of the
Department of Health and Human Services.
Many states have additional laws establishing obligations and penalties relating to the security and
privacy of patient information. For example, California law requires licensed healthcare facilities to
report breaches to the California Department of Public Health (CDPH) and to the affected patient(s)
within 15 business days of discovery.
Adventist Health privacy policies apply to ALL written, verbal, and electronic information.
Patient privacy and confidentiality are important to Adventist Health because:
• Patient confidentiality is essential to the development of trust between providers and patients.
• Patients have a legal right to control who sees, accesses or hears their protected health
information (PHI).
• Patients must be able to expect that information about their health is kept private, unless there
is a compelling reason that it should not be (i.e., for treatment, payment or healthcare
operations).
• Without patient privacy, patients would be hesitant to reveal sensitive information about
themselves.
• Volunteers, Providers, Contractors, Vendor Representatives and other Adventist Health
workforce members can be held personally liable for violating patient privacy laws. This includes
fines and penalties (e.g., jail time).
This means that communications with or about patients need to be kept private and limited to those
people who need to know the information for treatment, payment, or healthcare operations purposes
How the Laws Apply to Volunteers
22
Patient information that you see, hear, or read during the course of performing your duties, cannot be
shared with anyone unless the sharing of information is necessary to fulfill a job-related purpose and the
recipient has a job-related need to know. This includes your co-workers, other patients, visitors, your
family and friends, or anyone else who may ask you about information. Protecting patient information is
a responsibility that the entire workforce shares, including volunteers, regardless of whether you are
directly involved in the care of patients.
Social Media
Do not share any patient information on social media that is acquired through your work at Adventist
Health, even if the information is public.
• Posting patient information without appropriate authorization from the patient is a violation of
a patient’s right to privacy and confidentiality.
• Even if you do not include the name or other identifying information in your communication, it
still may be identifiable to others.
Protected Health Information (PHI)
PHI includes:
• Names
• Dates relating to a patient:
o birthdates
o dates of medical treatment
o admission and discharge dates
o dates of death
• Other:
o telephone numbers:
§ addresses (including city, county, or zip code)
§ fax numbers and other contact information
o Social Security numbers
o Medical records numbers
o Photographs
o Finger and voice prints
o Any other unique identifying number
o Bills
o Claims
o Prescriptions
o Data
o Lab results
o Medical opinions
o Appointment histories
Ways to Protect PHI
• Be aware of your surroundings.
• Keep information confidential.
• Do not share patient information with unauthorized individuals, even if the information is de-
identified.
• Do not view information out of curiosity or concern.
• Do not post patient information of any kind on social media.
23
• Lock computer screens when left unattended.
• Verify patient identifiers prior to mailing patient information to ensure that it gets to the right
person at the right place.
• Do not leave patient information on answering machines.
• Dispose of PHI only in appropriate shred bins, not regular trash cans.
Patient Rights
We must all work to honor and protect the privacy of our patients and to protect the confidentiality and
integrity of our patient’s protected health information. It is professional practice, but it is also federal
and state law.
Consequences of Noncompliance
Adventist Health has a workforce sanction policy for members of our workforce who violate patient
privacy and privacy/security policies.
Potential civil and criminal penalties for violating HIPAA privacy or security rules, may include large fines
and up to 10 years in prison.
These penalties can be levied against you, as well as Adventist Health.
Reporting Violations
Volunteers must strive to act ethically, comply with all laws and regulations, and immediately
report any violations or suspected violations. If you have any questions, suspect, or want to
report a violation of this Policy, contact your local compliance officer; the Corporate Compliance
Executive or the Office of General Counsel (OGC) in Roseville at 1-916-406-2000; or anonymously
report to the Compliance Hotline at 1-888-366-3833.
Hospital Safety
Handwashing
Hand washing and clean hands are the most significant means of preventing the spread of infection
from one person to another. Proper hand hygiene can reduce the number of nosocomial infections (a
nosocomial infection is an infection that was not present in the patient at the time of admission but was
acquired during their hospital stay).
Removing germs through hand washing or by using a hospital approved foam or hand gel is vital
protection against many types of infection. Always perform hand hygiene before and after you have
contact with a patient or anything a patient has touched. Wearing gloves does not replace hand
hygiene. In order to provide a safe hospital environment, hand hygiene must be practiced faithfully by
all hospital personnel, including volunteers, without exception as follows:
• When you arrive at AHGL.
• Before and after touching a patient or a patient’s belongings.
24
• Before you eat, apply cosmetics, handle contact lenses, or smoke. Eating, drinking, applying
makeup (including lip balm) and handling of contact lenses is prohibited in areas where
exposure to blood or other body fluids is likely.
• After using the restroom.
• After coughing or sneezing.
• After handling possibly contaminated articles such as blood tubes, culture plates, and trash.
• After removing personal protective equipment such as gloves, gowns, etc.
• Before you leave the hospital.
Infection Control
If you are feeling ill, or have symptoms of respiratory or gastrointestinal infections, such as coughing,
sneezing, heavy nasal discharge, diarrhea, flu symptoms, or a rash, please stay home.
If you or another member of your household has a communicable disease such as measles, mumps,
chicken pox, German measles, shingles, hepatitis, mononucleosis, salmonella, tuberculosis or a disease
that you are not sure is communicable, please inform the Director of Volunteer Resources, and/or the
Employee Health Nurse and please stay home.
Infection Control is everybody’s business! All employees and volunteers play a vital role in the Infection
Control Program in preventing and controlling the spread of infections in the hospital setting. This is
accomplished through education and training, good work practices such as good hand washing, and
following policies for universal/standard precautions and other isolation/precaution policies.
Flu Season Every year AHGL employees and volunteers are vaccinated for the flu. Students, Interns, and
Volunteers are included in this requirement as well.
Pathogens
There are four types of pathogens (disease-causing germs) of major concern in the hospital environment
that if left unchecked pose a threat to our patients and to us:
1. Blood-borne pathogens
2. Droplet pathogens
3. Contact pathogens
4. Airborne pathogens
Bloodborne Pathogens
Blood-borne pathogens include such microorganisms (germs) as the AIDS virus (HIV), the hepatitis B
virus, and the hepatitis C virus (HCV). They are transmitted via the blood and other potentially
infectious materials (OPIM) such as semen, vaginal secretions, cerebrospinal fluid, synovial fluid,
pericardial fluid, peritoneal fluid, amniotic fluid, saliva in dental procedures, any body fluid that is visibly
contaminated with blood, and all body fluids where it is difficult or impossible to differentiate between
fluids.
Since we are not always able to identify patients infected with blood-borne diseases, the blood and
body fluids, excretions, secretions (except sweat), non-intact skin and mucous membranes of all patients
will be treated as though they are infected, whether or not they are. This is known as
Standard/Universal Precautions.
25
Droplet Pathogens
Droplet pathogens (disease-causing germs) are transmitted by large particle droplets that can be
generated by the patient during coughing, sneezing, talking, or the performance of procedures that
cause coughing (cough inducing).
Contact Pathogens
Contact pathogens (germs) are transmitted by direct or indirect contact with the patient, patient care
items or the patient environment.
Examples of a Contact Pathogen include MSRA (methicillin-resistant Staphylococcus aureus), VRE
(vancomycin-resistant Enterococcus) and Clostridium difficile diarrhea.
Airborne Pathogens
These pathogens are spread by very small particles called “droplet nuclei” that remain in and infect the
air. They can be carried by air currents over long distances.
Examples of an Airborne Pathogen include Tuberculosis (TB), measles, and varicella (chickenpox or
shingles).
PPE Protection
Personal Protective Equipment or PPE’s such as gloves, masks, goggles and sterile gowns, help to protect
you from the spread of infection by imposing a barrier between you and a potentially infectious
substance.
All hospital staff, including volunteers should:
• Wear gloves when it is likely that hands will be in contact with wet body substances (blood,
urine, feces, wound drainage, oral secretions, sputum, vomitus). Change gloves and wash hands
between each patient contact.
• Wear a personal protective gown when it is likely that clothing will be soiled with body
substance.
• Wear masks and/or eye protection if there is a chance that body substances might be splashed
or inhaled in to the mouth, nose, or eyes.
• Wash hands for 15 seconds after patient contact paying particular attention to the area around
fingernails and between fingers.
Volunteers MUST reporting to nursing station before entering patient rooms and wash hands.
Volunteer Safety
Rules help protect patients, visitors, employees and volunteers from known or anticipated hazards. The
best rule is to use good common sense and judgment while at the hospital in order to prevent incidents.
However, some specific rules are needed to draw attention to the various hazards that may be
encountered while volunteering.
• Know how to do your assignment properly and safely. Any suggestions as to better and safer
methods should be given to your supervisor.
• Wear special protective items such as gloves, face shields or goggles, conductive shoes, etc.
where there is a potential exposure to blood or bodily fluids. Wash hands immediately after
removing gloves.
26
• Practice good housekeeping by having a place for everything and keeping everything in its place
when not being used.
• Keep equipment, tools, materials and work areas clean and orderly.
• Walk. Do not run.
• Use handrails on stairs.
• Be cautious when approaching swinging doors, corners or congested areas.
Most back injuries result from improper lifting. Back injuries can affect more than job performance.
There may be an impact on every part of a person’s life –physical, social, and psychological. So it makes
sensed to learn about and use techniques that can protect your back. To use good body mechanics for
lifting you should:
• Size up the load before you lift. If it looks heavy, it probably is!
• Plan your route and make sure it is clear of obstacles.
• Get a firm footing. Spread your feet to shoulder width apart for a wide base of support and to
improve balance, pointing your toes outward. This allows your body to compensate for any
shifts in weight.
• Bend your knees to allow the stronger leg muscles to participate in lifting, more than the weaker
back muscles.
• Do not bend at the waist.
• Maintain a curve in your lower back to keep the spine in an optimal (neutral) position. Don’t
“round” your back.
• Keep the load close to your body. This improves balance and requires less muscle force for the
lift. It also decreases the stress to your spine.
• Never twist and lift. Turn with your feet first, rather than with your back. By twisting the spine,
you place an enormous stress on your lower back. Twisting injuries are a leading cause of
herniated discs.
Emergency Codes
CODE RED Fire. 3 chimes throughout the Hospital – 3 loud buzzing sounds – overhead page
announcing, “Code Red”. See following pages on how to proceed.
CODE BLUE Cardiopulmonary Arrest, Medical Emergency CPR Needed. 3 loud buzzing
sounds – overhead page announcing, “Code Blue”. Stay out of the way.
CODE WHITE Infant Medical Emergency. 3 loud buzzing sounds – overhead page announcing,
“Code White”. Stay out of the way.
CODE PINK Infant Abduction. 3 loud buzzing sounds – overhead page announcing, “Code
Pink”. Respond quickly by going to the closest outside door and standing in front
of it to not let anyone through that might be carrying a baby. Take note of any
individual walking out with an infant. Try to engage them in a conversation in
order to prevent them from leaving the premises. Do not physically stop the
27
person. Take a mental or written description of the individual and phone in
description to Security at extension 3166 or “0” if they walk out the door.
CODE PURPLE Child Abduction. Same as “Code Pink”.
CODE TRIAGE Disaster. 3 loud buzzing sounds – overhead page announcing, “Code Triage”.
This means a disaster has occurred. See below on how to proceed.
CODE YELLOW Bomb Threat. 3 loud buzzing sounds – overhead page announcing, “Code Yellow
in (area suspected)”. Stay away from the mentioned area! If you suspect a
bomb, call ext. 3333
CODE GRAY Physical help needed. Combative/disruptive person. 3 loud buzzing sounds –
overhead page announcing, “Code Gray in Room ___ or in the lobby/ER” (can be
anywhere in the hospital). Code Gray designates that a patient or visitor is out of
control and staff is needed for assistance. No need for you to respond.
CODE SILVER A person with a weapon in on site or there is a hostage situation. 3 loud
buzzing sounds – overhead page announcing, “Code Silver in ___”. Unless
otherwise instructed, volunteers should stay in his/her areas.
CODE ORANGE Hazardous Materials. 3 loud buzzing sounds – overhead page announcing,
“Code Orange in ___”. Stay away from the mentioned area! If you discover the
spill call ext. 3333.
CODE SILENT Cardiac arrest in ER. 3 loud buzzing sounds – overhead page announcing, “Code
Silent ER”. Unless otherwise instructed, stay in your area.
CODE TRIAGE EXTERNAL
An internal or external disaster where the hospital may be receiving numerous injured individuals as a
result of a train accident, school bus accident, earthquake, wildfire, flood, biological event, civil unrest,
etc.) Report to your area supervisor or designated meeting area and await instructions on how to be of
assistance. If you are at home –don’t tie up the phone lines! Initiate your family disaster plan, stay calm
and help others to do so. Watch TV or listen to the radio announcements from the hospital. All
available personnel, including volunteers will report to the Command Center for instructions on how to
be of assistance in the event of a true disaster.
CODE TRIAGE INTERNAL
An internal or external disaster (i.e., bomb threat, earthquake, power outage, chemical leak, riot, etc.)
Dial 6464 to report location of the disaster. All available personnel, including volunteers will report to
the Command Center for instructions on how to be of assistance in the event of a true disaster.
Fire Safety
Remember RACE:
R – Rescue and Remove all patients from the immediate area
28
A – Activate the nearest fire alarm. Call ext. 6464 to give necessary information (location, nature and
extent of fire)
C – Contain/Confine the fire by closing the doors
E – Evacuate everyone to a safe area
Remain calm, do not panic and act quickly.
How to Use a Fire Extinguisher (PASS)
While holding the fire extinguisher upright:
Pull pin
Aim at the base of the fire
Squeeze lever
Sweep side to side
Fire Extinguishers
• Trash, wood, paper – use a pressured water extinguisher (silver)
• Liquids, grease – smother or use dry chemical extinguisher (red)
• Electrical equipment – use multi-purpose dry chemical extinguisher
Look for the appropriate symbols (A, B, C) on your extinguisher
What Causes Fires
It is the responsibility of every employee and volunteer to be constantly aware of conditions that can
lead to or cause a fire and/or explosion. When fire strikes, the actions taken during the first few minutes
can make the difference. Fire is a chemical reaction involving rapid oxidation or burning of a fuel. It
needs three elements to occur: FUEL, OXYGEN, AND HEAT
• FUEL- Fuel can be any combustible material - solid, liquid or gas. Most solids and liquids become
a vapor or gas before they will burn.
• OXYGEN - The air we breathe is about 21 percent oxygen. Fire only needs an atmosphere with at
least 16% oxygen.
• HEAT- Heat is the energy necessary to increase the temperature of the fuel to a point where
sufficient vapors are given off for ignition to occur.
• CHEMICAL REACTION - A chain reaction can occur when the three elements of fire are present in
the proper conditions and proportions. Fire occurs when this rapid oxidation, or burning takes
place. Take any one of these factors away, and the fire cannot occur or will be extinguished if it
was already burning. All fires, including suspected and/or non-locatable or smoke must be
reported immediately without any need for authorization from your supervisor of anyone else.
Prevent Fires: Make it a habit to watch for fire hazards.
Important Points
When first starting out in your department, find out the following:
29
• Where is your Fire Manual located?
• Where is the nearest fire extinguisher and fire alarm?
• Where are your fire doors?
• Where is your emergency evacuation route?
Leave 18 inches of space between an item and the sprinkler head.
To put out a wastebasket fire, try to smother it by covering the basket. If that doesn’t work, use the
nearest fire extinguisher.
In case of an emergency, dial x6464 immediately!!
Fire Evacuation Routes/Procedures
Fire doors, corridors and stairs must always remain clear, unobstructed and free from storage to allow
safe evacuation during an emergency. There are always two different exit routes out of your work area
or floor. Evacuation Routes, corridors and stairwells are clearly marked by “EXIT” signs. Do not use
elevators during a fire. Use the stairs. In patient care areas, it is preferable to “defend-in-place” by
closing doors unless the fire or smoke is directly threatening patients. Once you close the door, DO NOT
re-enter the room. If evacuation is necessary, evacuate laterally by clearing the hallways by pushing
everything to one side. If you must leave the floor, try to go vertically down a few floors, but stay in the
building. Use your shirt as a filter and hold your breath as much as possible. Follow instructions from
supervisor. Make sure to reassure patients and visitors. Await further instructions.
If your clothing catches on fire, remember to STOP, DROP, and ROLL. Stop whatever you are doing, drop
to the floor and roll to smother the flames. If someone else’s clothing is on fire, wrap them in a rug or
blanket to smother the flames. Don’t try to remove any fabric that gets stuck to a burn. Cover is with a
loose, clean cloth and get immediate medical help.
Evacuation and Patient Priorities
After removing all persons from immediate danger, evacuate in the following order:
1) Ambulatory patients and guests
2) Wheelchair or minimally disabled
3) Non-ambulatory bedridden. Use Paraslyde evacuation devices if non-ambulatory patients must
be dragged down the stairs (available on every nursing unit).
4) Medical records –only if it is safe to do so
Disaster Plan Policy
At an AH Location
In the event a Location of Adventist Health (AH) is disrupted due to a disaster, each Location
has a disaster plan in place. Refer to your Location’s Disaster Plan for more information.
In the Community
In the event a disaster occurs in the community of an AH Location, which may involve people
rendered ill or injured and in need for immediate medical care, refer to your Location’s Disaster
Plan. One of AH’s purpose is always to be ready to meet the needs of its’ community in the event of
a disaster. Each employee is part of an organized plan to help the Location Disaster Plan address
30
such emergencies. Check with your supervisor regarding your duties in the Location Disaster Plan. If
you can safely report to work, it is important that you report for your regularly scheduled shift
during a disaster or be ready to report if able for Disaster Duty if not regularly scheduled. Disaster
practice drills are held periodically to test each Location’s readiness.
Workplace Protocols
Abuse Recognition and Reporting
Every Volunteer has the obligation to look for, recognize, and report any suspected or actual abuse of
patients. The abuse may be child abuse, elder abuse, domestic violence, or assault.
The following conditions may alert you to the fact that abuse may be occurring:
• There is no explanation for the injury, or the explanation does not seem believable
• There has been a delay in seeking medical treatment
• The patient has a previous history of injuries or the injuries are in different stages of healing
• The patient’s behavior changes or is inappropriate when in the presence of family or significant
others
• Other family members do not allow the patient to speak for him or herself.
If you suspect or have knowledge of abuse to a patient, please contact your supervisor.

31
Health Requirements
I. PPD tuberculosis (TB) skin test done within 3 months of
application date. If history of positive PPD: Copy of chest x-ray
results done within 3 years of actual start date.
II. Proof of appropriate immunizations (i.e., MMR-Measles, mumps,
and rubella)
III. Varicella titer (only if you have had Chicken Pox) or immunization
if you desire to work with children.
IV. TDAP Vaccination within 10 years of start.
V. 10 Panel Urine Drug Screen (Negative) within 3 months of start.
VI. Influenza Vaccine Seasonal (October 01-March 31)
VII. Covid-19 Vaccination + Booster (Copy of card required

32
Campus Map
Volunteer Services
Department
